Should hypothyroidism during pregnancy be treated?

Pregnancy causes many changes in a woman’s body. One of these changes is the levels of various hormones produced by the body.
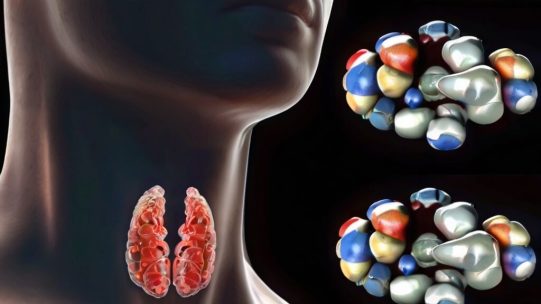
In the case of thyroid-stimulating hormone (TSH), pregnant women produce lower than normal levels (0.4 to 4.0 milli international units per liter). Some international guidelines recommend that levels not exceed 2.5 to 3 milli international units per liter during pregnancy; if TSH levels rise above this level, it can lead to subclinical hypothyroidism, or mild hypothyroidism, which, if left untreated, can cause many health problems If left untreated, it can cause a number of health problems.
Today, Mayo Clinic researchers report that one of the consequences may be loss of pregnancy. In addition, the researchers suggest a measure that could have a positive impact on as many as 15 out of 100 pregnancies: in a study published in the BMJ, they show that treating subclinical hypothyroidism (not quite to the level of treating it in women who are not pregnant) can reduce pregnancy loss, especially in those with TSH levels at or above the upper limit of normal. They show that treating subclinical hypothyroidism (not to the level treated in non-pregnant women) can reduce pregnancy loss, especially in those with TSH levels at or above the upper limit of normal.
A recent analysis of 18 studies showed that pregnant women with untreated subclinical hypothyroidism are at increased risk for pregnancy loss, placental abruption, premature rupture of membranes, and neonatal death,” says Spyridoula Maraka, MD, endocrinologist and lead author of the study. It seemed that treating subclinical hypothyroidism would reduce the likelihood of such fatalities.” However, we know that treatment poses other risks.
Using the OptumLabs data warehouse, Dr. Maraka’s team studied the health information of 5,405 pregnant women diagnosed with subclinical hypothyroidism. Of these, 843 women with an average pre-treatment TSH concentration of 4.8 milli-international units per liter were treated with thyroid hormone therapy. The remaining 4,562 had a mean pre-treatment TSH concentration of 3.3 milli international units per liter and were not treated.
Compared to the untreated group, the treated women were 38% less likely to experience pregnancy loss. However, they were more likely to experience preterm labor, gestational diabetes, and preeclampsia.
The team also looked at pre-treatment TSH levels to see if there was a time when treatment had the best overall effect.
Surprisingly, we found that women with pre-treatment TSH levels as high as 4.1 to 10 milli international units per liter benefited the most from treatment,” says Dr. Maraka. ‘This group was much less likely to experience pregnancy loss, which allowed us to lower their average levels.’
The researchers found that in women with low levels of TSH (2.5 to 4.0 milli international units per liter), the risk of gestational hypertension (which can lead to preeclampsia) was significantly higher in treated women than in untreated women. women with TSH (4.1 to 10 milli international units) did not differ between treated and untreated women who had higher levels of TSH (4.1 to 10 milli international units per liter).
The study was conducted by the Mayo Clinic,” said Juan Brito Campana, M.D., an endocrinologist at the Mayo Clinic and a co-author of the study. If TSH levels are in the range of 2.5 to 4.0 [milli international units per liter], subclinical hypothyroidism may be best left untreated.”
The researchers found no other adverse outcomes that might be affected by differences in pre-treatment TSH levels or subsequent thyroid hormone use.
Dr. Brito Campana added that the association between levothyroxine therapy (a drug used to treat hypothyroidism) and risk of pregnancy-related adverse outcomes (e.g., preeclampsia and gestational diabetes) should be viewed as a preliminary finding and that additional studies evaluating the safety of levothyroxine therapy in pregnant women with subclinical hypothyroidism The authors state that the association with risk of adverse pregnancy outcomes (e.g., preeclampsia and gestational diabetes) should be viewed as preliminary findings and that additional studies should be sought to evaluate the safety of levothyroxine therapy in pregnant women with subclinical hypothyroidism. The study’s findings and recommendations seem somewhat prophetic: on January 6, 2017, the American Thyroid Association released its latest care guidelines, which include treatment recommendations for women who experience thyroid disease during pregnancy.
“These guidelines help women and their doctors decide together what is best for them,” says Dr. Brito.
“We are pleased to see them and remain committed to further medical research and refinement of available information to support shared decision-making and improved health.”